
Osteoarthritis of the ankle joint — degenerative-dystrophic damage to the cartilage tissue. But since the articular surfaces of the bones are involved in the process as the disease progresses, it is more correct to call it arthrosis. In foreign literature, when describing this disease, the term osteoarthritis is used, which indicates not only degenerative changes, but also inflammation of this background.
Osteoarthritis — This is a chronic, progressive joint disease in which cartilage, joint surfaces of bones, capsule and periarticular tissues are destroyed. This leads to pain and impaired joint mobility. The ankle rarely suffers from osteoarthritis, unlike the knee. The disease occurs more often in women over 50 years of age and in athletes who have suffered leg injuries. In case of arthrosis of the ankle joint, the treatment depends on the manifestations of the disease and is selected individually by an orthopedic traumatologist. Doctors use methods that have proven their effectiveness and safety, and practice a multidisciplinary approach to treat the problem and prevent the progression of joint pathology.
This article is advisory in nature. Treatment is prescribed by a specialist after consultation.
How the disease develops
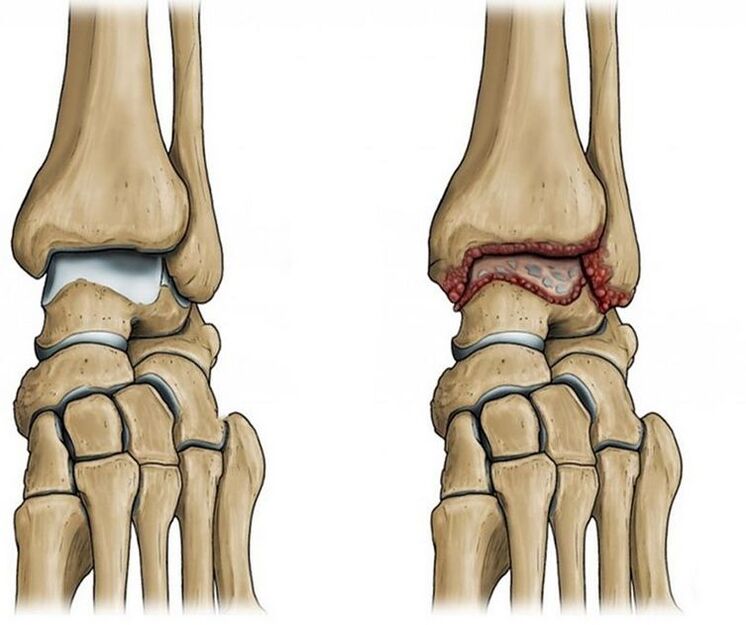
The ankle joint is formed by three bones: the tibia, fibula and talus, covered by a joint capsule and reinforced by ligaments. Thanks to the work of the muscles, the foot bends and unfolds. Normally, the articular surfaces are smooth and slide easily against each other during movements. Covered with dense, elastic cartilage, its main function is to protect the bones and absorb the load. The joint cavity contains synovial fluid. It plays the role of intra-articular lubrication, preventing friction of the joint elements and their abrasion during movements.
But as a result of injury or natural aging of the joint, the joint surfaces become rough, and the cartilage tissue loses its smoothness and elasticity. When the cartilage is damaged and the degenerative changes progress, the bones begin to come into contact with each other during movement in the joint, which is accompanied by pain.
In attempts to "protect" and compensate for further damage to the joint and surrounding tissues, osteophytes are formed - growth on the edges of the joint surfaces of the bones. As a result, the mobility of the joint is partially or even completely limited.
Depending on the root cause, the following types of osteoarthritis are distinguished:
- Primary or idiopathic osteoarthritis. In this case, we are talking about degenerative-dystrophic changes in the joint
- Secondary is related to exposure to a specific causative factor, usually previous joint damage. And this form is most often diagnosed
Predisposing factors
The main predisposing factors for the development of arthrosis of the ankle joint:
- intra- and peri-articular injuries, such as bone fractures, tears and ligament tears
- ankle surgery
- inflammatory joint lesions in the past
- intense loads: professional sports, ballet, long walking, work related to long periods of "standing"
- sedentary way of life
- wearing high heels for a long time
- Overweight
- hereditary collagenopathies leading to impaired collagen synthesis
- chronic damage to joint structures due to excessive loads
- metabolic disorders: diabetes, gout
- estrogen deficiency in postmenopausal women
- rheumatic diseases
- foot deformities such as flat feet
- degenerative-dystrophic changes in the spine, complicated by the formation of an intervertebral hernia, which is accompanied by compression of the nerve root
Ankle arthrosis: symptoms
The main sign of arthrosis — Pain is what makes you seek help from a doctor. At the beginning of the development of the disease, the pain is unpleasant only after prolonged exertion and decreases with rest.
Depending on the stage of pathological changes in the joint, the pain becomes more intense and continues at rest and even at night. Other symptoms appear.
There are three stages of the disease:
- The first stage is characterized by slight swelling, redness of the skin of the joint area, pain in the afternoon or after intense physical exertion. Unpleasant sensations are localized on the front surface of the leg, along the line of the joint and move to the lateral surfaces of the ankle. X-ray of the leg may still show no changes.
- In the second stage, the pain becomes constant, there is a crunch when moving the joint, mobility is limited and the joint "gets stuck". An X-ray examination shows growths on the edges of the articular surfaces of the bones: tibia, ankles and talus, as well as a narrowing of the joint gap
- In the third stage, the joint is deformed, which is why only low-amplitude rocking movements are possible. Radiography reveals massive bony growths, the joint space is sharply narrowed or even absent. Due to instability of the joint, patients often twist their leg, which only worsens the situation due to sprains, torn ligaments and deterioration of the general condition
Pain with arthrosis of the ankle has characteristic features:
- Maximally expressed at the beginning of the movement — the so-called initial pain
- Significantly increases with load, especially when running, jumping
- It often occurs in the evening, at night or immediately after waking up
Due to pain, there is limited mobility of the foot as well as jamming in the joint as the cartilage breaks down.
Symptoms appear in waves: exacerbations alternate with remissions. In case of exacerbation, the symptoms are more pronounced. During remission, symptoms gradually subside and may even disappear completely.
Which doctor should I contact?
In the event of pain and stiffness in the movements of the ankle, you should consult an orthopedic traumatologist. If another cause of joint discomfort is found, consultation with a neurologist, rheumatologist or endocrinologist may be necessary.
Diagnosis
To make a diagnosis, the doctor clarifies the complaints, specifies how long the pain has been observed, which contributes to its appearance and intensification. The specialist collects data on existing diseases, injuries and lifestyle characteristics, conducts an examination, assesses the range of motion in the joint and performs diagnostic tests.
Already based on the information received, it is possible to assume a diagnosis, but in order to confirm and draw up a competent treatment plan, additional research methods are needed, which may include:
- X-ray of the ankle joint, which is of primary importance in establishing the diagnosis and determining the stage of development of the disease. Images show narrowing of the joint space, osteophytes along the edges of the articular surfaces of the bones, cysts, and signs of thinning of the bone underlying the cartilage
- Computed tomography of the joint reflects the picture in more detail. The doctor can assess in detail the condition of the patient's bone structures and cartilage tissue
- MRI is used to examine cartilage and soft tissue
- Ultrasound of a joint to assess the condition of the soft joint structures
Treatment of arthrosis
The treatment of the pathology is long-term and is carried out under the supervision of an orthopedic traumatologist on an outpatient basis. How to treat arthrosis of the foot depends on the stage of damage and existing complications.
The main goals of treatment of the disease in a modern clinic are to relieve pain in the legs, improve the patient's quality of life and slow down the progression of arthrosis. To do this, the doctor develops a set of therapeutic and preventive measures, drug and non-drug, and also adjusts the patient's lifestyle.
Adjustment of lifestyle and diet
Sufficient physical activity and correction of nutrition will help limit degenerative changes. After the examination, the doctors of the clinic can give recommendations for weight loss, as well as for optimizing the load on the legs.
Medication treatment
Medicines are selected individually based on examination data, symptoms and concomitant diseases. The patient may be prescribed:
- Analgesics. Most often, these are non-steroidal anti-inflammatory drugs in the form of tablets, gels, injections to relieve pain and inflammation.
- Antidepressants and anticonvulsants for prolonged, severe, intractable pain
Exercise therapy
Specially selected exercises help maintain the range of motion in the joint, reduce pain and limit the progression of degenerative changes. The patient performs the recommended exercises first under the supervision of a specialist, and then on his own at home.
Massage
Massage of the lower limb normalizes the nutrition of joint tissues. It is prescribed outside the acute stage. During the session, the specialist performs passive movements in the joint, which prevents shortening of the muscles and stiffness of the joint.
Assistive devices
Special orthoses, canes, and walkers may be recommended to relieve stress and stabilize the ankle joint.
surgery
It is used only in case of severe destruction of the articular cartilage and limited mobility of the joint. After the operation, there is a long period of rehabilitation and conservative treatment. Endoprosthetics or endoprosthetics in the later stages of ankle arthrosis — practically the only option to avoid damage and maintain joint mobility.
Why is ankle arthrosis dangerous?
Already formed changes in the joint are irreversible. Therefore, treatment is aimed at slowing down the pathological process in order to preserve the patient's ability to work and quality of life. Achieving such goals is possible only with timely treatment and strict adherence to the doctor's recommendations.
With the development of arthrosis, a pronounced deformation of the joint is formed. The range of motion is sharply reduced, as a result, the ability to support the leg becomes difficult, walking without crutches or a cane is almost impossible.
Chronic, persistent joint pain leads to anxiety and depressive disorders.
Prevention
Prevention of arthrosis includes the following measures:
- Avoid traumatic activities. For example, jumping from a great height, running
- Avoid injury
- Be careful in icy conditions, wear non-slip shoes
- Control your body weight
- Normalizing body weight will help reduce stress on the ankle joint
- Stay moderately active
- An inactive lifestyle is dangerous and leads to complications, as well as overuse and micro-injuries
- Keep your joints healthy
- Consult a doctor in a timely manner and treat diseases of the musculoskeletal system
Highlights of the article:
- The prevalence of degenerative-dystrophic diseases of the joints of the legs is 87%
- Occupational risks, daily habits and past injuries can lead to osteoarthritis of the ankle joint.
- A common symptom of arthrosis — pain that is accompanied by crunching when moving, local swelling and later limited mobility of the leg
- Treatment of ankle arthrosis is often conservative and includes both drug and non-drug methods.
- The progression of arthrosis of the ankle leads to damage and complete loss of function of the foot























